Reference Publications
Below, please find assay references from our instructions for use documents. Don’t see what you’re looking for? Contact Us
IHC General Publications
Useful Publications for all IHC Assays
- Kiernan JA. Histological and Histochemical Methods: Theory and Practice. New York: Pergamon Press 1981.
- Sheehan DC and Hrapchak BB. Theory and Practice of Histotechnology. St. Louis: C.V. Mosby Co. 1980.
- Nadji M, Morales AR. Immunoperoxidase, part I: the techniques and its pitfalls. Lab Med. 1983; 14:767-771.
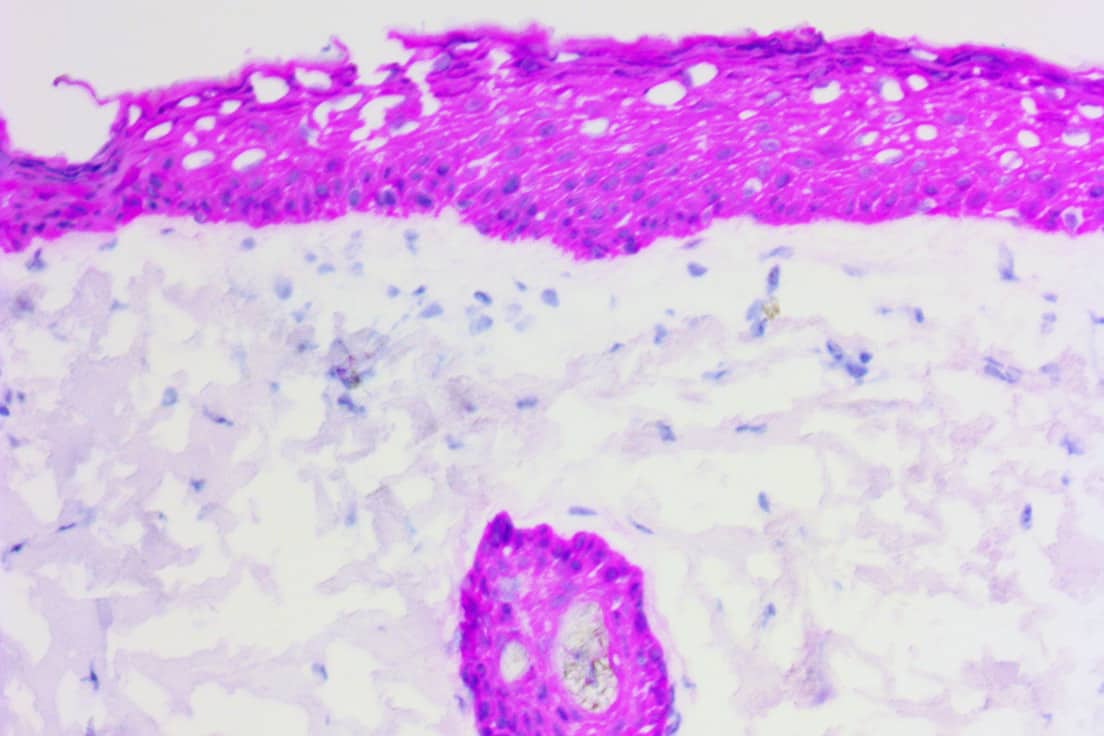
AE1/AE3
- Woodcock-Mitchell J, Eichner R, et al. Immunolocalization of Keratin Polypeptides in Human Epidermis Using Monoclonal Antibodies. The Journal of Cell Biology. November 1982; 95:580-588.
- Weiss RA, Eichner R, et al. Monoclonal Antibody Analysis of Keratin Expression in Epidermal Diseases: A 48- and 56-kdalton Keratin as Molecular Markers for Hyperproliferative Keratinocytes. The Journal of Cell Biology. April 1984; 98:1397-1406.
- Moll R, Divo M, et al. The human keratins: biology and pathology. Histochem Cell Biol. 2008; 129:705–733.
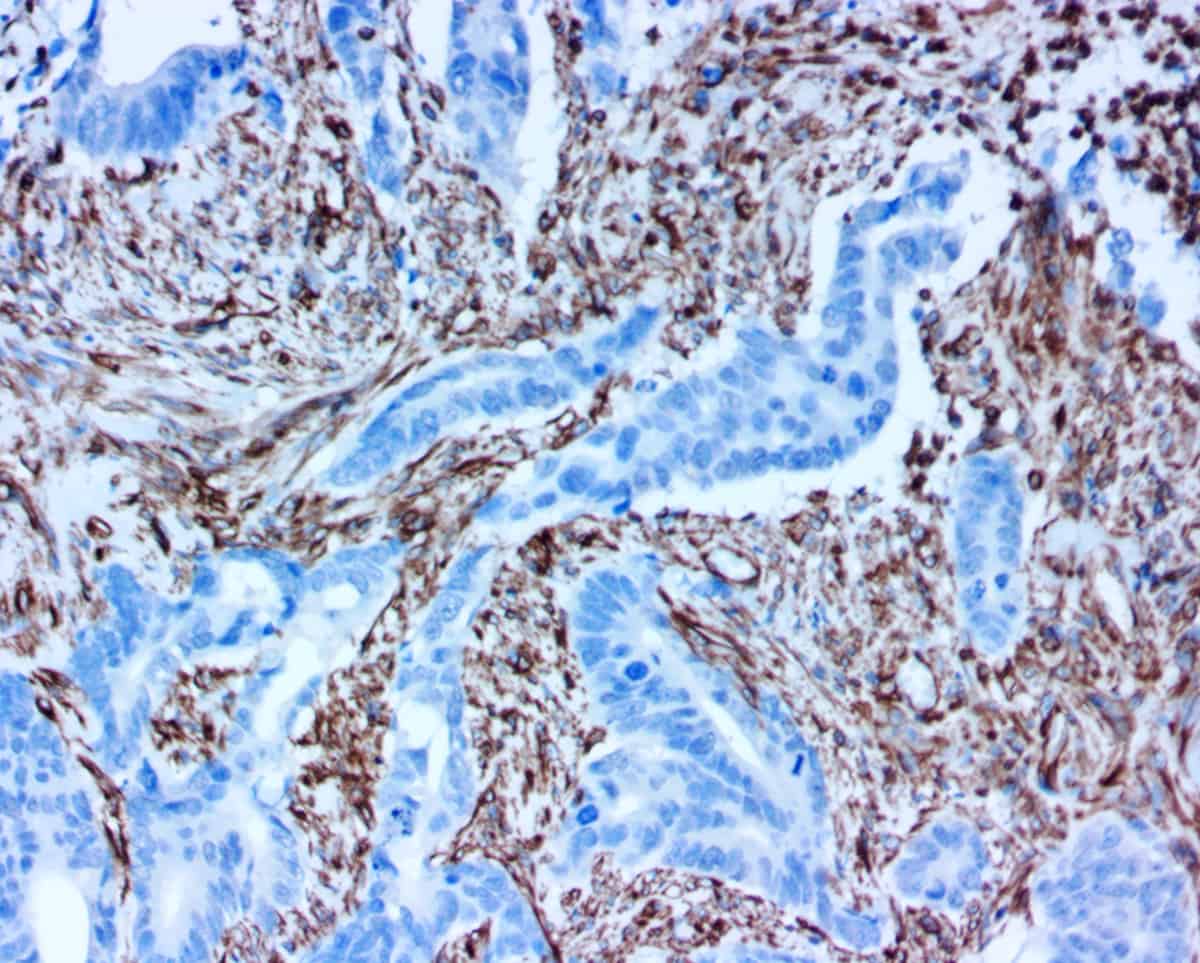
Calponin
- Gusev NB. Some properties of caldesmon and calponin and the participation of these proteins in regulation of smooth muscle contraction and cytoskeleton formation. Biochemistry (Mosc). 2001 Oct; 66(10):1112-21.
- Douglas-Jones A et al. Observer variability in the histopathological reporting of core biopsies of papillary breast lesions is reduced by the use of immunohistochemistry for CK5/6, calponin and p63. Histopathology 2005, 47, 202-08.
- Abdallah DM and El Deeb NMF. Comparative Immunohistochemical Study of P63, SMA, CD10 and Calponin in Distinguishing In Situ from Invasive Breast Carcinoma. J Mol Biomark Diagn. 2017, 8(4), 1000342.
- Perez-Montiel MD et al. Differential Expression of Smooth Muscle Myosin, Smooth Muscle Actin, H-Caldesmon, and Calponin in the Diagnosis of Myofibroblastic and Smooth Muscle Lesions of Skin and Soft Tissue. Am J Dermatopathol. 2006 Apr;28(2):105-11.
CD20
- Chang KL, Arber DA, Weiss LM. CD20: A review. Applied Immunohistochemistry 1996; 4:1-15.
- Jaffe ES, et al. WHO Classification of Tumours. Pathology and Genetics of Tumours of Haematopoietic and Lymphoid Tissues. Lyon, IARC Press 2001.
- Jilani I, et al. Transient down-modulation of CD20 by rituximab in patients with chronic lymphocytic leukemia. Blood. 2003 Nov; 102(10):3514-20.
- Khalidi HS, et al. The immunophenotype of blast transformation of chronic myelogenous leukemia: a high frequency of mixed lineage phenotype in “Lymphoid” blasts and A comparison of morphologic, immunophenotypic, and molecular findings. Mod Pathol. 1998 Dec; 12:1211-21.
CD34
- Gardner LJ., Evaluation of bone marrow specimens with acute myelogenous leukemia for CD34, CD15, CD117 and myeloperoxidase, Arch Pathol Lab Med. 2001 Aug;125(8):1063-9.
- Flint A., Weiss, S.W., CD34 and Keratin Expression Distiguishes Solitary Fibrous Tumor (Fibrous Mesothelioma) of Plera from Desmoplastic Mesothelioma, Hum Pathol. 1995 Apr; 26(4):428-31.
- Hoang, M.P. et al. CD34 expression in desmoplastic melanoma, J Cutan Pathol. 2001 Nov;28(10):508-12.
- Hao, X, et al. Dermatofibrosarcoma Protuberans: Update on the Diagnosis and Treatment, J Clin Med 2020 Jun; 9(6): 1752.
CD45
- Krishna M. Diagnosis of Metastatic Neoplasms. Arch Pathol Lab Med. 2010; 134:207–215.
- Andres TL, Kadin ME. Immunologic Markers in the Differential Diagnosis of Small Round Cell Tumors from Lymphocytic Lymphoma and Leukemia. Am J Clin Pathol 1983; 79:546-552.
- Thunnissen E, Flieder DB, et al. The Use of Immunohistochemistry Improves the Diagnosis of Small Cell Lung Cancer and Its Differential Diagnosis. An International Reproducibility Study in a Demanding Set of Cases. Journal of Thoracic Oncology. 2017; Vol. 12 No. 2: 334-346.
CDX2
- Saad RS, et al. Usefulness of Cdx2 in separating mucinous bronchioloalveolar adenocarcinoma of the lung from metastatic mucinous colorectal adenocarcinoma. Am J Clin Pathol. 2004; 122:421-7.
- Kaimaktchiev V, et al. The homeobox intestinal differentiation factor CDX2 is selectively expressed in gastrointestinal adenocarcinomas. Mod Pathol. 2004; 17:1392-9.
- Werling RW, et al. CDX2, a highly sensitive and specific marker of adenocarcinomas of intestinal origin: an immunohistochemical survey of 476 primary and metastatic carcinomas. Am J Surg Pathol. 2003; 27:303-10.
- Groisman GM, et al. The value of Cdx2 immunostaining in differentiating primary ovarian carcinomas from colonic carcinomas metastatic to the ovaries. Int J Gynecol Pathol. 2004; 231:52-7.
- Moskaluk CA, et al. Cdx2 protein expression in normal and malignant human tissues: an immunohistochemical survey using tissue microarrays. Mod Pathol. 2003; 16:913-9.
CEA
- Berretta M, Alessandrini L, et al. Serum and tissue markers in colorectal cancer: State of art. Critical Reviews in Oncology/Hematology. 2017; 111:103–116.
- Tiernan JP, Perry SL, et al. Carcinoembryonic antigen is the preferred biomarker for in vivo colorectal cancer targeting. Br J Cancer. 2013 Feb 19; 108 (3):662–667.
- Wu K-L, Huang E-Y, et al. Synergistic interaction between galectin-3 and carcinoembryonic antigen promotes colorectal cancer metastasis. Oncotarget. 2017; Vol. 8, No. 37: 61935-61943.
Chromogranin A
- O’Connor DT. Chromogranin: widespread immunoreactivity in polypeptide hormone producing tissues and in serum. Regul Pept. 1983 Jul;6(3):263-80.
- Hendy GN et al. Chromogranin A. Clin Invest Med. 1995; 18(1): 47-65.
- Gut P, Czarnywojtek A, & Fischbach J et al. Chromogranin A – unspecific neuroendocrine marker. Clinical utility and potential diagnostic pitfalls. Arch Med Sci. 2016 Feb 1; 12(1): 1–9.
- Torske KR et al. Adenoma versus carcinoid tumor of the middle ear: a study of 48 cases and review of the literature. Mod Pathol. 2005; 15(5): 543-55
- Louthan O, Chromogranin A in Physiology and Oncology. Folia Biologica (Praha) 2011;57:173-18.
CK5
- Moll R, et al. Expression of keratin 5 as a distinctive feature of epithelial and biphasic mesotheliomas. An immunohistochemical study using monoclonal antibody. Virchows Arch B Cell Pathol. 1989; 58:129-45.
- Ordonez NG. What are the current best immunohistochemical markers for the diagnosis of epithelioid mesothelioma? A review and update. Human Pathology. 2007; 38:1–16.
CK 7
- Montezuma D, et al. A panel of four immunohistochemical markers (CK7, CK20, TTF-1, and p63) allows accurate diagnosis of primary and metastatic lung carcinoma on biopsy specimens. Virchows Arch. 2013 Dec; 463(6):749-54.
- Shin JH, et al. CK7, CK20, CDX2 and MUC2 Immunohistochemical staining used to distinguish metastatic colorectal carcinoma involving ovary from primary ovarian mucinous adenocarcinoma. Jpn J Clin Oncol. 2010 Mar;40(3):208-13.
- Lambaudie E, et al. Cytokeratin 7 as a predictive factor for response to concomitant radiochemotherapy for locally advanced cervical cancer: a preliminary study. Anticancer Res. 2014, Jan; 34(1): 177-81.
CK 8/18
- Cimpean AM et al. Relevance of the immunohistochemical expression of cytokeratin 8/18 for the diagnosis and classification of breast cancer. Romaniam Journal of Morphology and Embryology. 2008; 49(4):479-483.
- Reisenblichler ES et al. The predicative ability of a CK5/p63/CK8/18 antibody cocktail in stratifying breast papillary lesions on needle biopsy. Am J Clin Pathol. 2013; 140:767-779.
CK 19
- Jerome Marson V et al. Expression of TTF-1 and cytokeratins in primary and secondary epithelial lung tumours: correlation with histological type and grade. Histopathology. 2004; 45(2): 125-34.
- Stroescu C., et al. The diagnostic value of cytokeratins and carcinoembryonic antigen immunostaining in differentiating hepatocellular carcinomas from intrahepatic cholangiocarcinomas. J Gastrointesin Liver Dis., 2006;(1): 9-14.
- Durnez A. et al. The clinicopathological and prognostic relevance of cytokeratin 7 and 19 expression in hepatocellular carcinoma. A possible progenitor cell origin. Histopathology. 2006; 49(2)L 138-5
- Maki M et al. Expression of cytokeratin 1, 5, 14, 19 and transforming growth factors-beta1, beta2, beta3 in osteofibrous dysplasia and adamantinoma: A possible association of transforming growth factor-beta with basal cell phenotype promotion. Pathol Int. 2000; 50(10): 801-7.
CK 20
- Chu PG et al. Immunohistochemical staining in the diagnosis of pancreatobiliary and ampulla of Vater adenocarcinoma: application of CDX2, CK17, MUC1, and MUC2. Am J Surg Pathol. 2005; 29(3): 359-67.
- McGregor DK et al. Reduced expression of cytokeratin 20 in colorectal carcinomas with high levels of microsatellite instability. Am J Surg Pathol. 2004; 28(6): 712-8.
- Terracciano LM et al. Hepatoid adenocarcinoma with liver metastasis mimicking hepatocellular carcinoma: an immunohistochemical and molecular study of eight cases. Am J Surg Pathol. 2003; 27(10): 1302-12.
E-Cadherin
- Wong SHM, et al. E-cadherin: Its dysregulation in carcinogenesis and clinical implications. Crit Rev Oncol Hematol. 2018 Jan;121:11-22.
- Van Roy F. Beyond E-cadherin: roles of other cadherin superfamily members in cancer. Nat Rev Cancer.
EMA
- Nassar H. et al. Pathogenesis of invasive micropapillary carcinoma: role of MUC1 glycoprotein. Mod Pathol. 2004 Sep; 17(9):1045-50.
- Acs G, et al. Invasive ductal carcinomas of the breast showing partial reversed cell polarity are associated with lymphatic tumor spread and may represent part of a spectrum of invasive micropapillary carcinoma. Am J Surg Pathol. 2010 Nov; 34(11):1637-46.
- Mino-Kenudson M, et al. Mucin expression in reactive gastropathy: an immunohistochemical analysis. Arch Pathol Lab Med. 2007 Jan; 131(1):86-90.
- Kadin ME, et al. Primary cutaneous ALCL with phosphorylated/activated cytoplasmic ALK and novel phenotype: EMA/MUC1+, cutaneous lymphocyte antigen negative. Am J Surg Pathol. 2008 Sep; 32(9):1421-6.
- Kuan SF, et al. Differential expression of mucin genes in mammary and extramammary Paget’s disease. Am J Surg Pathol. 2001 Dec; 25(12):1469 77.
EpCAM
- Ge W et al. A Novel Molecular Signature of Cancer-Associated Fibroblasts Predicts Prognosis and Immunotherapy Response in Pancreatic Cancer. Int J Mol Sci 24:N/A (2022).
- Rickstrew J, Neill B, Wong CM, Tolkachjov SN. Use of anti-epithelial cell adhesion molecule (EpCAM) immunostain for histologic evaluation of aggressive basal cell carcinomas during Mohs micrographic surgery. Int J Dermatol. 2024 Apr;63(4):530-531. doi: 10.1111/ijd.17025. Epub 2024 Jan 18. PMID: 38238815.
- Sen S, Carnelio S. Expression of epithelial cell adhesion molecule (EpCAM) in oral squamous cell carcinoma. Histopathology. 2016 May;68(6):897-904. doi: 10.1111/his.12870. Epub 2015 Nov 16. PMID: 26401964.
ER
- Staebler A,Hormone receptor immunohistochemistry and human papillomavirus in situ hybridization are useful for distinguishing endocervical and endometrial adenocarcinomas, Am J Surg Pathol 2002;26:998.
- Mohsin SK, Weiss H, et al. Progesterone receptor by immunohistochemistry and clinical outcome in breast cancer: a validation study, Mod Pathol 2004;17:1545.
Galectin-3
- Sumana BS, et al. Galectin-3 immunohistochemical expression in thyroid neoplasms. J Clin Diag Res. 2015 Nov; 9(11): ec07-ec11.
- Cvejic DS, et al. Galectin-3 expression in papillary thyroid carcinoma: Relation to histomorphologic growth pattern, lymph node metastasis, extrathyroid invasion, and tumor size. Head Neck. 2005 Dec; 27(12):1049-55.
- Savin S, et al. Thyroid peroxidase and galectin-3 immunostaining in differentiated thyroid carcinoma with clinicopathologic correlation. Human Pathology 39(11) Nov 2008, 1656-1663.
- Rossi ED, et al. Diagnostic and prognostic role of HBME-1, Galectin-3, and β- Catenin in poorly differentiated and anaplastic thyroid carcinomas. Appl Immunohistochem Mol Morphol 2013 May; 21(3):237–41.
GFAP
- Eng LF et al. Glial Fibrillary Acid Protein: GFAP-Thirty-One Years (1969- 2000) Neurochemical Res. 2000, 25(9/10):1439-1451.
- Jessen KR et al. Molecular identity, distribution and heterogeneity of glial fibrillary acidic protein: an immunoblotting and immunohistochemical study of Schwann cells, satellite cells, enteric glia and astrocytes. J Neurocytol. 1984 Apr; 13(2):187-200.
- Roessmann U et al. Glial fibrillary acidic protein (GFAP) in ependymal cells during development: an immunocytochemical study. Brain Res. 1980; 200(1):13-21.
- O’Callaghan JP and Sriram K. Glial fibrillary acidic protein and related glial proteins as biomarkers of neurotoxity. Expert Opin Drug Saf. 2005 May; 4(3): 433-442.
HER2
- Calhoun BC and Collins LC: Predictive markers in breast cancer: An update on ER and HER2 testing and reporting; Semin Diagn Pathol 2015 Sep;32(5):362-9.
- Ridolfi, RL,ER-2/neu testing in breast carcinoma: a combined immunohistochemical and fluorescence in situ hybridization approach, Mod Pathol. 2000 Aug;13(8):866-73.
Ki67
- Goodson WH 3rd, et al. The functional relationship between in vivo bromodeoxyuridine labeling index and Ki67 proliferation index in human breast cancer. Breast Cancer Res Treat. 1998 May; 49(2): 155-164.
- Scholzen T, Gerdes J. The Ki-67 protein: from the known and the unknown [review]. J Cell Physiol. 2000; 182:311-22.
- Lohmann CM, et al. Expression of melanocyte differentiation antigens and ki-67 in nodal nevi and comparison of ki-67 expression with metastatic melanoma. Am J Surg Pathol. 2002 Oct; 26(10):1351-7.
Mart-1
- Cheraghi N et al. Melanoma Treated With Mohs Micrographic Surgery Using a Novel-Modified 15-Minute MART-1 Immunostain: Discussion of Technique and Experience. Dermatol Surg 2020;00:1-3
- Kageshita T et al. Differential expression of Mart-1 in primary and metastatic melanoma lesions. J Immunother. 1997; 20:460-5
- Orchard GE. Melan A (Mart-1): a new monoclonal antibody for malignant melanoma diagnosis. Br J Bioed Sci 1998 Mar; 55(1): 9-9
Napsin A
- Brasch F et al. Involvement of napsin A in the C- and N-terminal processing of surfactant protein B in type-Il pneumocytes of the human lung. J Biol Chem. 2003;278:49006-49014.
- Bishop JA et al. Napsin A and thyroid transcription factor-I expression in carcinomas of the lung, breast, pancreas, colon, kidney, thyroid, and malignant mesothelioma. Hum Pathol. 2010;41:20-25.
- Turner BM et al. Napsin A, a new marker for lung adenocarcinoma, is complementary and more sensitive and specific than thyroid transcription factor I in the differential diagnosis of primary pulmonary carcinoma: evaluation of 1674 cases by tissue microarray. Arch Pathol Lab Med. 2012; 136: 163—171.
- Rekhtman N, et al. Pulmonary large cell neuroendocrine carcinoma with adenocarcinoma-like features: Napsin A expression and genomic alterations. Mod Pathol. 2018 Jan; 31(1): 1 1 1-121.
p40
- Boonen, M, et al. A Dileucine Signal Situated in the C-terminal Tail of the Lysosomal Membrane Protein p40 Is Responsible for Its Targeting to Lysosomes. Biochem J. 2008 Sep 15;414(3):431-40.
- Liu, Y. et al. ∆Np63/p40 Correlates With the Location and Phenotype of basal/mesenchymal Cancer Stem-Like Cells in Human ER+ and HER2+ Breast Cancers, J Pathol Clin Res. 2020 Jan;6(1): 83-93.
- Leinard, D, et al. Vaccination of Melanoma Patients with Melan-A/Mart-1 Peptide and Klebsiella Outer Membrane Protein p40 as an Adjuvant. J Immunother. 2009 Oct;32(8):875-83.
- Sato, H, et al. Measles Virus N Protein Inhibits Host Translation by Binding to eIF3-p40: J Virol. 2007 Nov;81(21):11569-76.
p120
- Kourtidis A, Ngok SP, Anastasiadis PZ. p120 catenin: an essential regulator of cadherin stability, adhesion-induced signaling, and cancer progression. Prog Mol Biol Transl Sci. 2013;116:409-432. doi:10.1016/B978-0-12-394311-8.00018-2.
Pan-CK 4Abs
- Woodcock-Mitchell J, Eichner R, et al. Immunolocalization of Keratin Polypeptides in Human Epidermis Using Monoclonal Antibodies. The Journal of Cell Biology. November 1982; 95:580-588.
- Weiss RA, Eichner R, et al. Monoclonal Antibody Analysis of Keratin Expression in Epidermal Diseases: A 48- and 56-kdalton Keratin as Molecular Markers for Hyperproliferative Keratinocytes. The Journal of Cell Biology. April 1984; 98:1397-1406.
- Moll R, Divo M, et al. The human keratins: biology and pathology. Histochem Cell Biol. 2008; 129:705–733.
- Ordonez NG. What are the current best immunohistochemical markers for the diagnosis of epithelioid mesothelioma? A review and update. Human Pathology. 2007; 38:1–16.
Podoplanin
- Ugorski M et al. Podoplanin – a small glycoprotein with many faces. Am J. Cancer Res. 2016;6(2):370-386.
- Breiteneder-Geleff S et al. Angiosarcomas express mixed endothelial phenotypes of blood and lymphatic capillaries: podoplanin as a specific marker for lymphatic endothelium. Am J Pathol. 1999 Feb; 154(2):385-94.
- Astarita JL et al. Podoplanin: emerging functions in development, the immune system, and cancer. Frontiers in Immunology. 2012 Sep; 283(3):1- 11.
PR
-
Arnedos M, Nerurkar P, et al.Discordance between core needle biopsy (CNB) and excisional biopsy (EB) for estrogen receptor (ER), progesterone receptor (PgR) and HER2 status in early breast cancer (EBC), Ann Oncol 2009;20:1948..
- Mohsin SK, Weiss H, et al. Progesterone receptor by immunohistochemistry and clinical outcome in breast cancer: a validation study, Mod Pathol 2004;17:1545.
PRAME
- Ikeda, H, et al. Characterization of an antigen that is recognized on a melanoma showing partial HLA loss by CTL expressing an NK inhibitory receptor”. Immunity. 6(2) 1997: 199–208.
- Kirkin, AF, et al. The immunogenic properties of melanoma-associated antigens recognized by cytotoxic T lymphocytes. Experimental and Clinical Immunogenetics. 15(1): 19–32.
- Matsushita, M, et al. Preferentially expressed antigen of melanoma (PRAME) in the development of diagnostic and therapeutic methods for hematological malignancies”. Leukemia & Lymphoma. 44(3): 439–44.
PTH
- Matsushita H, Usui M, Hara Y, et al: Co-Secretion of parathyroid hormone and parathyroid-hormone-related protein via a regulated pathway in human parathyroid adenoma cells. Am J Pathology 1997;150(3):661-871 2.
- Oka T, Yoshioka T, Shrestha GR, et al: Immunohistochemical study of nodular hyperplastic parathyroid glands in patients with secondary hyperparathyroidism. Virchows Archive A 1988;413(1):53-60 3.
- Wick MR, Ritter JH, Humphrey PA, Nappi O. Clear cell neoplasms of the endocrine system and thymus. Semin Diagn Pathology 1997;14(3):183-20.
SMMS-1
- Kalof AN et al. Immunostaining patterns of myoepithelial cells in breast lesions: a comparison of CD10 and smooth muscle myosin heavy chain. J Clin Pathol. 2004; 57: 625-629.
- Hill CB, Yeh IT. Myoepithelial cell staining patterns of papillary breast lesions: from intraductal papillomas to invasive papillary carcinomas. AM J Clin Pathol. 2005 123(1) 36-44.
SOX10
- Miettinen M et al. Sox10 – A marker for not only Schwannian and melanocytic neoplasms but also myoepithelial cell tumors of soft tissue. A systematic analysis of 5134 tumors. Am J Surg Pathol. 2015 June; 39(6) 826-835.
- Buonaccorsi JN et al. Diagnostic utility and comparative immunohisto-chemical analysis of MITF-1 and SOX10 to distinguish melanoma in situ and actinic keratosis: a clinicopathological and immunohistochemical study of 70 cases. Am J Dermatopathol. 2014 Feb; 36(2): 124-30.
- Kang Y et al. Diagnostic utility of SOX10 to distinguish malignant peripheral nerve sheath tumor from synovial sarcoma, including intraneural synovial sarcoma. Mod Pathol. 2014 Jan; 27(1): 55-61.
Synaptophysin
- Sidiropoulos M et al. Expression of TdT in Merkel cell carcinoma and small cell lung carcinoma. Am J Clin Pathol. 2011; 135(6): 831-8.
- Kwon SE et al. Synaptophysin regulates the kinetics of synaptic vesicle endocytosis in central neurons. Neuron. 2011; 70(5): 847-54.
- Miller DC et al. Synaptophysin: a sensitive and specific marker for ganglion cells in central nervous system neoplasms. Hum Pathol. 1990; 21(3): 271-6.
TPO
- Thyroid peroxidase and galectin-3 immunostaining in differentiated thyroid carcinoma with clinicopathologic correlation. Hum Pathol. 2008 Nov;39(11):1656-63.
- Zeiger MA, Dackiw AP: Follicular thyroid lesions, elements that affect both diagnosis and prognosis. J Surg Oncol. 2005 Mar 1;89(3):108-13.
- Weber, K B et al., The Use of a Combination of Galectin-3 and Thyroid Peroxidase for the Diagnosis and Prognosis of Thyroid Cancer. Am J Clin Pathol 2004;122:524-531.
- Yousaf U et al. Immunohistochemical staining for thyroid peroxidase (TPO) of needle core biopsies in the diagnosis of scintigraphically cold thyroid nodules, Clin Endocrinol, 2008 Jun; 68(6): 996-1001.
TROP2
- Liu H. et al. The Potential Diagnostic Utility of TROP-2 in Thyroid Neoplasms, Applied Immunohistochemistry & Molecular Morphology. 2017. 25 (8):525-533.
- Shvartsur A, Bonavida B. TROP2 and its overexpression in cancers: regulation and clinical/therapeutic implications. Genes -105 & Cancer. 2015. 6(34):84.
- McDougall RA, Tolcos M et al. TROP2: From Development to Disease. Developmental Dynamics. 2015. 244:99-109.
TTF1
- Ulici V., Wang LJ. TTFI. PathologyOutlines.com website. http://www.patholoeyoutlines.com/topic/stainsttfl.html ..
- Misch D., et al. Value of thyroid transcription factor (TTF)-I for diagnosis and prognosis of patients with locally advanced or metastatic small cell lung cancer. Diagn Pathol. 2015; 10:2 1 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4391673/.
- Cardnell R., et al Protein expression of TTFI and cMYC define distinct molecular subgroups of small cell lung cancer with unique vulnerabilities to aurora kinase inhibition, DLL3 targeting, and other targeted therapies. Oncotarget.8 201 7: 73419-73432. https://www.oncotarget.eom/article/20621/text/.
Vimentin
- Azumi N, Battifora H. The distribution of vimentin and keratin in epithelial and nonepithelial neoplasms. A comprehensive immunohistochemical study on formalin and alcohol-fixed tumors.Am J Clin Pathol.1987; 88:286-96.
- Khoury JD, et al. The utility of epithelial membrane antigen and vimentin in the diagnosis of chromophobe renal cell carcinoma.Ann Diagn Pathol.2002; 6(3):154-58.
- Hermann H, Aebi U. Intermediate filaments and their associations: multitalented structural elements specifying cytoarchitecture and cytodynamics. Curr Opin Cell Biol. 2000; 12:79-90..
- Niveditha SR, Bajaj P. Vimentin expression in breast carcinomas. Indian J Pathol Microbiol. 2003; 46(4):579-84..
WT1
- Proc Natl Acad Sci U S A. 2010 Aug 3;107(31):13824-9, PMID: 20631300; Cell. 1993 Aug 27;74(4):679-91, PMID: 8395349;
- Sexual Development. 2007;1(4):238-54, PMID: 18391535; Oncologist. 2012;17(2):250-9, PMID: 22291091; BMC Cancer. 2006 Apr 11;6:90, PMID: 16606472
- Dao T, Yan S, Veomett N, et al. Targeting the intracellular WT1 oncogene product with a therapeutic human antibody. Sci Transl Med. 2013;5(176):176ra33. doi:10.1126/scitranslmed.3005661.
Still have questions?
If you couldn't find what you were looking for and still have questions, don't hesitate to reach out.
Contact Us